Beyond Muscle: The Complex Story of Cellular Growth in Health and Disease
- Apr 3, 2025
- 6 min read
Updated: Apr 6, 2025

In the fitness world, "hypertrophy" has become a buzzword plastered across workout plans and supplement labels. But this term—alongside its lesser-known and contentiously debated counterpart "hyperplasia"—represents sophisticated biological processes with implications far beyond building biceps.
Hypertrophy is defined as "the enlargement of an organ or tissue from the increase in size of its cells", it is not simply restricted to the realms of the muscular system - that is just myo-hypertrophy (a muscle growth response to stimuli like resistance training which can be either myofibrillar (increased muscle proteins) or sarcoplasmic (increased fluid within the muscle cell).
As health professionals, understanding these cellular mechanisms provides critical insight way beyond just muscular development and reaches into everything from weight management to cardiovascular health and ageing.
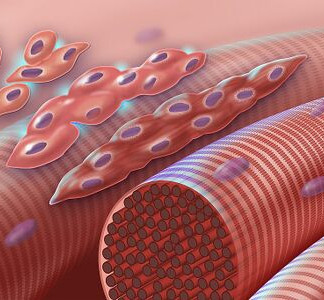
The Cellular Language of Growth
At its core, for now, our discussion centres on two distinct growth mechanisms:
Hypertrophy: The enlargement of existing cells
Hyperplasia: The increase in cell number through division
While seemingly straightforward, these processes manifest differently across tissues, with profound implications for health and disease. Let's consider the impact on our fat cells...
Adipose Tissue: A Tale of Two Growth Patterns
Perhaps nowhere is the distinction between hypertrophic and hyperplastic growth more clinically relevant than in adipose tissue. When we gain weight, our fat cells respond in one of two ways:
Hypertrophic Obesity
In hypertrophic obesity, existing adipocytes enlarge to accommodate increased triglyceride storage. This pattern presents several metabolic disadvantages:
Enlarged adipocytes become insulin resistant more readily
They secrete higher levels of pro-inflammatory cytokines
They exhibit reduced adiponectin production
They experience increased mechanical stress and are more prone to hypoxia
Research shows that individuals with predominantly hypertrophic obesity typically experience worse metabolic outcomes, including higher risks of insulin resistance, dyslipidaemia, and systemic inflammation. A 2019 study in the Journal of Clinical Investigation demonstrated that adipocyte size, independent of total fat mass, predicted insulin sensitivity and metabolic risk.
Simply put, having larger fat cells, rather than just more fat, is linked to poorer metabolic health.
Hyperplastic Obesity
Conversely, hyperplastic obesity involves the generation of new fat cells. While excess adiposity remains problematic, this pattern demonstrates several relative advantages:
New adipocytes tend to maintain better insulin sensitivity
They produce healthier adipokine profiles
They have improved vascular networks
They show enhanced capacity for healthy lipid storage
This helps explain why some individuals with obesity, often those with early-onset weight gain and predominantly hyperplastic patterns (more common in women and certain age brackets and cultures), maintain relatively better metabolic health despite higher BMI.
Important note: Whilst growing more fat cells (rather than enlarging existing ones) appears to be metabolically healthier - currently however, adult hyperplastic obesity is not widely accepted as a common adaptation, and is mostly observed in specific populations like children, pregnant women, and certain cultural groups. This is supported by research indicating:
Age-related decline in adipogenesis (Physiological Reviews: "Regulation of Adipogenesis" - https://journals.physiology.org/doi/full/10.1152/physrev.00015.2014)
The prevalence of hyperplasia in early-onset obesity (International Journal of Obesity: "Adipose tissue cellularity in human obesity" - https://www.nature.com/articles/0802100)
The unique adipocyte dynamics during pregnancy (PMC: "Adipose Tissue Remodeling During Pregnancy and Lactation" - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3227914/).
Adipose Tissue Fibrosis
Excessive accumulation of extracellular matrix (ECM) components within adipose tissue. Essentially, the scarring or stiffening of fat tissue, often associated with adipocyte hypertrophy, chronic inflammation, and metabolic stress...

See... "Hypertrophy isn't always the goal, especially if we widen our lens beyond the horizon of just skeletal muscles. It can lead to significant metabolic issues, including insulin resistance, inflammation, harmful fat tissue stiffening (adipose tissue fibrosis), and much more."
Cardiac Implications: When Growth Turns Pathological
The heart provides another compelling example of how cellular growth patterns influence health outcomes. Cardiac myocytes respond to different stimuli through distinct hypertrophic pathways:
Physiological Cardiac Hypertrophy
Endurance exercise induces what's termed "eccentric hypertrophy," characterised by:
Proportional growth in chamber size and wall thickness
Enhanced mitochondrial function
Improved calcium handling
Minimal fibrosis
Preserved or enhanced contractility
This adaptation supports increased stroke volume and cardiac output during exercise.
Pathological Cardiac Hypertrophy
In contrast, conditions like hypertension or aortic stenosis trigger "concentric hypertrophy":
Disproportionate increase in wall thickness
Shift towards glucose metabolism
Impaired mitochondrial function
Increased fibrosis
Re-expression of foetal gene programmes
Eventual progression to heart failure
The difference illustrates how the same cellular process—hypertrophy—can be adaptive or maladaptive depending on context and signalling pathways.
Muscle Preservation: Strategies Against Atrophy
Understanding hypertrophic mechanisms becomes particularly relevant when we consider sarcopenia—the age-related loss of muscle mass and function that affects approximately 10% of adults over 60 and 50% of those over 80.
Sarcopenia's impact extends far beyond aesthetics, with comorbidities including:
Increased fall risk and fracture rates
Impaired glucose metabolism and insulin resistance
Reduced basal metabolic rate
Compromised immune function
Diminished quality of life and independence
Higher all-cause mortality
Evidence-Based Interventions for Muscle Preservation
Current research supports several well supported and widely popularised strategies to combat sarcopenia and promote healthy myocyte hypertrophy:
1. Progressive Resistance Training
The foundation of any anti-sarcopenia programme. Key principles include:
Progressive overload (consistently increasing resistance)
Multi-joint compound movements
Training to momentary muscular failure in the 8-12 repetition range
2-3 sessions per week with 48-72 hours between targeting the same muscle groups
Emphasis on eccentric (lowering) phase of movements
A 2020 meta-analysis in Medicine & Science in Sports & Exercise demonstrated that progressive resistance training could increase muscle mass by 1.1 kg on average over 20.5 weeks in adults over 60.
2. Protein Optimisation
Current evidence suggests:
Total daily intake of 1.2-1.6g/kg body weight for older adults
Leucine-rich sources (dairy, whey, eggs, meat)
Even distribution across meals (25-30g per meal)
Pre-sleep casein protein may offer additional benefits
Protein intake within 2 hours post-exercise optimises MPS (muscle protein synthesis)
3. Other Nutritional Considerations
Vitamin D supplementation when levels are below 30ng/ml
Creatine monohydrate (3-5g daily)
Omega-3 fatty acids for their anti-inflammatory effects
Adequate overall caloric intake
Limiting alcohol consumption
Addressing micronutrient deficiencies
4. Hormonal Optimisation
Regular assessment of thyroid function
Monitoring of testosterone levels in men
Evaluation of growth hormone/IGF-1 axis
Management of insulin sensitivity
5. Lifestyle Factors
Prioritising sleep quality and quantity
Stress management
Avoiding prolonged periods of inactivity
Maintaining cardiovascular fitness
The Interconnected Cellular Ecosystem
What makes this topic so fascinating—and so relevant to comprehensive health practitioners—is the interconnection between these cellular processes across different tissues. Consider these relationships:
Muscle-Fat Crosstalk: Myokines released from active muscle tissue influence adipocyte metabolism and can promote "browning" of white adipose tissue.
Immune Regulation: Both adipocytes and muscle cells secrete cytokines that modulate systemic inflammation, which in turn affects cardiac health.
Neural Factors: Neurogenic atrophy triggers different signalling pathways than disuse atrophy, requiring distinct intervention strategies.
Metabolic Integration: Mitochondrial health within hypertrophied cells determines whether growth patterns will be sustainable or pathological.
Vascular Adaptation: Cellular hypertrophy requires concomitant angiogenesis to maintain adequate perfusion—a process that fails in certain pathological states.
This interconnection explains why isolated approaches focusing solely on one tissue often yield disappointing results. A person might build impressive muscle mass while harbouring metabolically dysfunctional adipocytes, or maintain a "healthy" BMI while experiencing cardiac remodelling due to untreated hypertension.
Clinical Applications: Beyond Buzzwords
For health practitioners, these concepts have immediate practical applications:
Assessment Refinement: Looking beyond simple metrics like BMI or muscle mass to consider functional capacity, adipocyte size distribution, inflammatory markers, and tissue quality.
Intervention Specificity: Tailoring exercise prescriptions based on the specific type of cellular adaptation desired (e.g., eccentric vs. concentric loading for different cardiac adaptations).
Nutritional Precision: Recognising how macronutrient timing and composition differently affect hyperplastic versus hypertrophic processes.
Medication Awareness: Understanding how common pharmaceuticals (especially statins, beta-blockers, and corticosteroids) influence tissue-specific growth patterns.
Monitoring Evolution: Tracking markers that indicate whether cellular growth is following adaptive versus maladaptive pathways.
The Future of Cellular Optimisation
Emerging research is revealing even more nuanced aspects of cellular growth regulation, with promising applications that go beyond our health and fitness industry scope of practice, however being aware of the advancements in this field are part of any dedicated professionals responsibility and so here are a few 'on-the-cusp' developments from neighbouring industries:
Exosome Therapy: Using cell-derived vesicles to deliver growth signals with high specificity
Time-Restricted Feeding: Leveraging circadian biology to optimise anabolic/catabolic cycles
Targeted Exercise Prescriptions: Using specific movement patterns to preferentially activate pathways that promote healthy cellular adaptation
Pharmacological Selectivity: Developing compounds that can stimulate beneficial hypertrophy while inhibiting pathological growth
Genetic Profiling: Identifying individuals predisposed to specific growth patterns and tailoring interventions accordingly
Conclusion: Reclaiming Cellular Wisdom
The reduction of complex biological terms like "hypertrophy" to fitness jargon represents more than semantic imprecision—it reflects a broader tendency to oversimplify the sophisticated systems we aim to optimise.
As integrative health practitioners, we have both the opportunity and responsibility to deepen our understanding of these mechanisms. This means moving beyond simplistic models of "gains" and "losses" toward a more nuanced appreciation of tissue-specific adaptations and their systemic implications.
By reclaiming the depth and precision of terms like hypertrophy and hyperplasia, we honour the complexity of the human body while enhancing our ability to facilitate positive adaptations across multiple physiological systems. This more sophisticated understanding allows us to support not only aesthetic goals and performance metrics but also functional capacity, metabolic health, and ultimately, longevity.
The cellular conversation happening within our bodies speaks a language of remarkable subtlety. As practitioners, our effectiveness depends on how fluently we can interpret this language—and how precisely, timely and consistently we can respond.
This article represents current understanding based on available research as of 2024.
As with all areas of medical and exercise science, recommendations may evolve as new evidence emerges.


.png)











Comments